 In a recent decision, the Louisiana Court of Appeal, Fourth Circuit, overturned a trial court ruling in a medical malpractice case involving the death of Nicole Phillips. The case, Jamal Wright et al. v. The State of Louisiana, O/B/ of Jamie Alleyn, M.D., et al., highlights the critical importance of adhering to proper service of process procedures when suing state-employed healthcare providers.
In a recent decision, the Louisiana Court of Appeal, Fourth Circuit, overturned a trial court ruling in a medical malpractice case involving the death of Nicole Phillips. The case, Jamal Wright et al. v. The State of Louisiana, O/B/ of Jamie Alleyn, M.D., et al., highlights the critical importance of adhering to proper service of process procedures when suing state-employed healthcare providers.
The case originated from a medical malpractice claim against several doctors employed by the State of Louisiana. The claim was initially brought before a medical review panel in 2015 and subsequently amended following the death of Nicole Phillips in 2016. The lawsuit was then filed by Jamal Wright, the father of Ms. Phillips’ minor child.
The Doctors, upon being served with the Petition for Damages, filed declinatory exceptions of insufficiency of citation and insufficiency of service of process. They argued that the service was improper as it was not directed to the designated agents for service of process as required by Louisiana law.
 Louisiana Personal Injury Lawyer Blog
Louisiana Personal Injury Lawyer Blog


 A recent Louisiana
A recent Louisiana  In a recent decision, the
In a recent decision, the  Providing sufficient expert testimony can be crucial to prevailing a medical malpractice lawsuit. But what happens when the court determines that the expert testimony offered by a doctor on the plaintiff’s behalf is insufficient because the doctor does not specialize in the same field as the defendant?
Providing sufficient expert testimony can be crucial to prevailing a medical malpractice lawsuit. But what happens when the court determines that the expert testimony offered by a doctor on the plaintiff’s behalf is insufficient because the doctor does not specialize in the same field as the defendant?  Undergoing a surgery is always a nerve-wracking experience. You want to be able to trust that your surgeon conducted and reviewed the appropriate pre-operative tests. Can a surgeon be held liable if he or she fails to review the results of the pre-operative tests before performing the surgery?
Undergoing a surgery is always a nerve-wracking experience. You want to be able to trust that your surgeon conducted and reviewed the appropriate pre-operative tests. Can a surgeon be held liable if he or she fails to review the results of the pre-operative tests before performing the surgery?  If the trial court does not rule in your favor, you might find yourself considering filing an appeal. However, just like filing an initial lawsuit, there are strict time limits for filing an appeal. If you do not comply with these time limits, the appellate court will be unable to consider the merits of your appeal, and you will be stuck with the trial court’s ruling.
If the trial court does not rule in your favor, you might find yourself considering filing an appeal. However, just like filing an initial lawsuit, there are strict time limits for filing an appeal. If you do not comply with these time limits, the appellate court will be unable to consider the merits of your appeal, and you will be stuck with the trial court’s ruling.  In the face of the profound loss that accompanies the passing of a family member, the impact can be particularly agonizing when that loss follows the anticipation of medical intervention, such as a transplant. The immediate inclination might be to explore legal avenues through a medical malpractice claim, yet the determination of whether negligence played a role can be an intricate matter for the average individual. This Louisiana case shows how important it can be to obtain expert testimony to help show malpractice occurred.
In the face of the profound loss that accompanies the passing of a family member, the impact can be particularly agonizing when that loss follows the anticipation of medical intervention, such as a transplant. The immediate inclination might be to explore legal avenues through a medical malpractice claim, yet the determination of whether negligence played a role can be an intricate matter for the average individual. This Louisiana case shows how important it can be to obtain expert testimony to help show malpractice occurred. 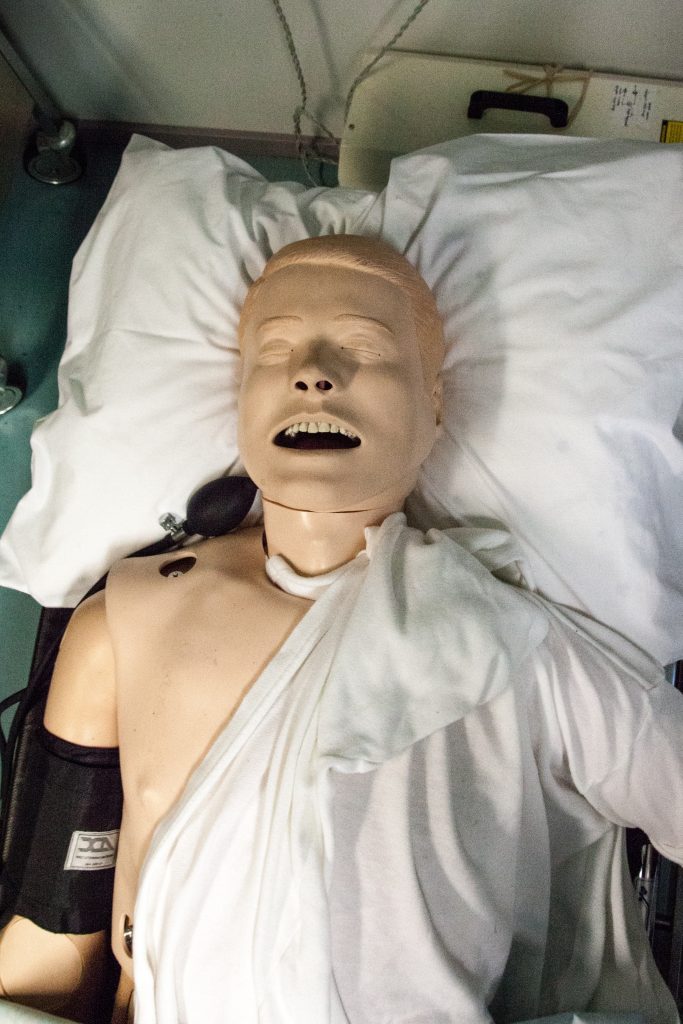 The prospect of undergoing medical procedures carries inherent risks; sometimes, unfortunate incidents can lead to injuries. In such cases, individuals can pursue medical malpractice claims to seek compensation for damages. A crucial aspect of these claims is presenting the appropriate evidence and adhering to procedural requirements. A telling illustration of the importance of these procedures is found in a lawsuit involving Elliott R. James and Lakeview Medical Center, LLC. This case underscores the significance of following legal protocols and obtaining substantial evidence to bolster a medical malpractice claim.
The prospect of undergoing medical procedures carries inherent risks; sometimes, unfortunate incidents can lead to injuries. In such cases, individuals can pursue medical malpractice claims to seek compensation for damages. A crucial aspect of these claims is presenting the appropriate evidence and adhering to procedural requirements. A telling illustration of the importance of these procedures is found in a lawsuit involving Elliott R. James and Lakeview Medical Center, LLC. This case underscores the significance of following legal protocols and obtaining substantial evidence to bolster a medical malpractice claim. When medical emergencies strike, the rapid response of emergency medical technicians (EMTs) can mean the difference between life and death. However, the high-pressure nature of their role can also give rise to complex legal questions when outcomes take a tragic turn. Richard Miller’s case sheds light on the intricate landscape of EMT liability, illuminating the balance between legal protections afforded to these healthcare professionals and the pursuit of justice for patients and their families. It also helps answer the question: Can an emergency medical technician or their employer be held liable when things go wrong?
When medical emergencies strike, the rapid response of emergency medical technicians (EMTs) can mean the difference between life and death. However, the high-pressure nature of their role can also give rise to complex legal questions when outcomes take a tragic turn. Richard Miller’s case sheds light on the intricate landscape of EMT liability, illuminating the balance between legal protections afforded to these healthcare professionals and the pursuit of justice for patients and their families. It also helps answer the question: Can an emergency medical technician or their employer be held liable when things go wrong?  In the realm of medical malpractice, the intricacies of the legal process can often appear daunting, especially when juxtaposed against the heart-wrenching backdrop of a stillborn baby’s tragedy. K Arceneaux found herself entangled in this very confluence of circumstances, seeking justice for her devastating loss while grappling with legal procedure demands. As the mother’s quest for accountability unfolds, a crucial question emerges: Can a plaintiff prevail in a medical malpractice case without the indispensable backing of expert testimony?
In the realm of medical malpractice, the intricacies of the legal process can often appear daunting, especially when juxtaposed against the heart-wrenching backdrop of a stillborn baby’s tragedy. K Arceneaux found herself entangled in this very confluence of circumstances, seeking justice for her devastating loss while grappling with legal procedure demands. As the mother’s quest for accountability unfolds, a crucial question emerges: Can a plaintiff prevail in a medical malpractice case without the indispensable backing of expert testimony?