 When receiving medical care, the choice of medical professional can influence your treatment. If you have been injured on the job, you might not be sure if you can pick your own doctor or if you have to use a doctor your employer selects. Under the Louisiana Workers’ Compensation Act, an injured worker is entitled to select a physician in any specialty for an initial visit. The employer is not required to approve the employee’s choice of physician. What happens if the employer claims the employee was not injured on the job?
When receiving medical care, the choice of medical professional can influence your treatment. If you have been injured on the job, you might not be sure if you can pick your own doctor or if you have to use a doctor your employer selects. Under the Louisiana Workers’ Compensation Act, an injured worker is entitled to select a physician in any specialty for an initial visit. The employer is not required to approve the employee’s choice of physician. What happens if the employer claims the employee was not injured on the job?
Blann Kyle filed a workers’ compensation claim against Boise Cascade Company (“Boise”), claiming he had lost his hearing as a result of his employment at a paper mill located in DeRidder, Louisiana. He filed the claim seven years after he retired. Kyle then filed a motion for an expedited hearing, under La. R.S. 23:1121. Kyle claimed Boise had not authorized his initial visit with his choice of physician. Kyle wanted the workers’ compensation judge to order Boise to authorize his initial visit to the physician he had selected, reimburse him for the medical expenses resulting from the testing and treatment by that physician, and pay penalties and attorneys’ fees. Boise countered that Kyle’s claims were prescribed, meaning he had waited too long to bring his workers’ compensation claim. Boise also claimed it was not proper for Kyle to request penalties and attorneys’ fees with his motion for an expedited hearing. The workers’ compensation judge denied Kyle’s motion, holding there was a “tenuous link” between Kyle’s alleged hearing loss and his employment. Therefore, Boise had acted properly in refusing him the choice of a physician. Kyle filed an appeal.
Louisiana courts have recognized that hearing loss can be caused by occupational exposure and can be an occupational disease where an injured worker is entitled to workers’ compensation. See Arrant v. Graphic Packaging International, Inc. Under La. R.S. 23:1121, an injured worker is entitled to select a physician in any specialty without his employer’s approval. If the employer denies that, the employee has the right to request an expedited proceeding. The employee can also receive attorney’s fees and penalties.
 In a significant victory for the family of a deceased worker, the Louisiana Court of Appeal has overturned a previous ruling, ensuring they receive workers’ compensation death benefits. The case, Orozco v. Filser Construction & Aries Building Systems, Inc., centered around the complex issue of determining whether Serna Jr. was an independent contractor or an employee entitled to workers’ compensation benefits.
In a significant victory for the family of a deceased worker, the Louisiana Court of Appeal has overturned a previous ruling, ensuring they receive workers’ compensation death benefits. The case, Orozco v. Filser Construction & Aries Building Systems, Inc., centered around the complex issue of determining whether Serna Jr. was an independent contractor or an employee entitled to workers’ compensation benefits. Louisiana Personal Injury Lawyer Blog
Louisiana Personal Injury Lawyer Blog


 Navigating the workers’ compensation system can be overwhelming when you’ve been injured on the job. You may be tempted to accept a quick settlement to cover immediate medical bills and lost wages. However, it’s crucial to understand the long-term implications of such a decision. A recent Louisiana case highlights the importance of carefully considering settlement agreements in workers’ compensation claims.
Navigating the workers’ compensation system can be overwhelming when you’ve been injured on the job. You may be tempted to accept a quick settlement to cover immediate medical bills and lost wages. However, it’s crucial to understand the long-term implications of such a decision. A recent Louisiana case highlights the importance of carefully considering settlement agreements in workers’ compensation claims. A recent
A recent  In today’s interconnected world, it’s not uncommon for employees to find themselves working across state lines. But what happens when an injury occurs in a different state than where the employment contract was formed? Whose laws apply? Can an injured worker sue their employer, or are they limited to workers’ compensation benefits? These questions were at the heart of the recent case
In today’s interconnected world, it’s not uncommon for employees to find themselves working across state lines. But what happens when an injury occurs in a different state than where the employment contract was formed? Whose laws apply? Can an injured worker sue their employer, or are they limited to workers’ compensation benefits? These questions were at the heart of the recent case  Contracting and subcontracting in the construction industry are standard practices. However, they can create several challenges when a worker is injured. What happens, for instance, when the employee of a subcontractor is injured by a device owned and operated by a municipal government unconnected to the construction project at hand? The Louisiana First Circuit Court of Appeal recently addressed this question when a worker was injured by an overhead power line.
Contracting and subcontracting in the construction industry are standard practices. However, they can create several challenges when a worker is injured. What happens, for instance, when the employee of a subcontractor is injured by a device owned and operated by a municipal government unconnected to the construction project at hand? The Louisiana First Circuit Court of Appeal recently addressed this question when a worker was injured by an overhead power line.  When an employee suffers a work injury, it may result in negative consequences for the employee’s health. While Louisiana’s workers’ compensation laws allow the employee to recover damages for these future health complications, this has its limits. The employee must prove that this future negative consequence was related to the initial injury at work. This ensures that employees who are rightfully harmed are compensated while also protecting businesses from having to pay for every future medical problem the employee has.
When an employee suffers a work injury, it may result in negative consequences for the employee’s health. While Louisiana’s workers’ compensation laws allow the employee to recover damages for these future health complications, this has its limits. The employee must prove that this future negative consequence was related to the initial injury at work. This ensures that employees who are rightfully harmed are compensated while also protecting businesses from having to pay for every future medical problem the employee has.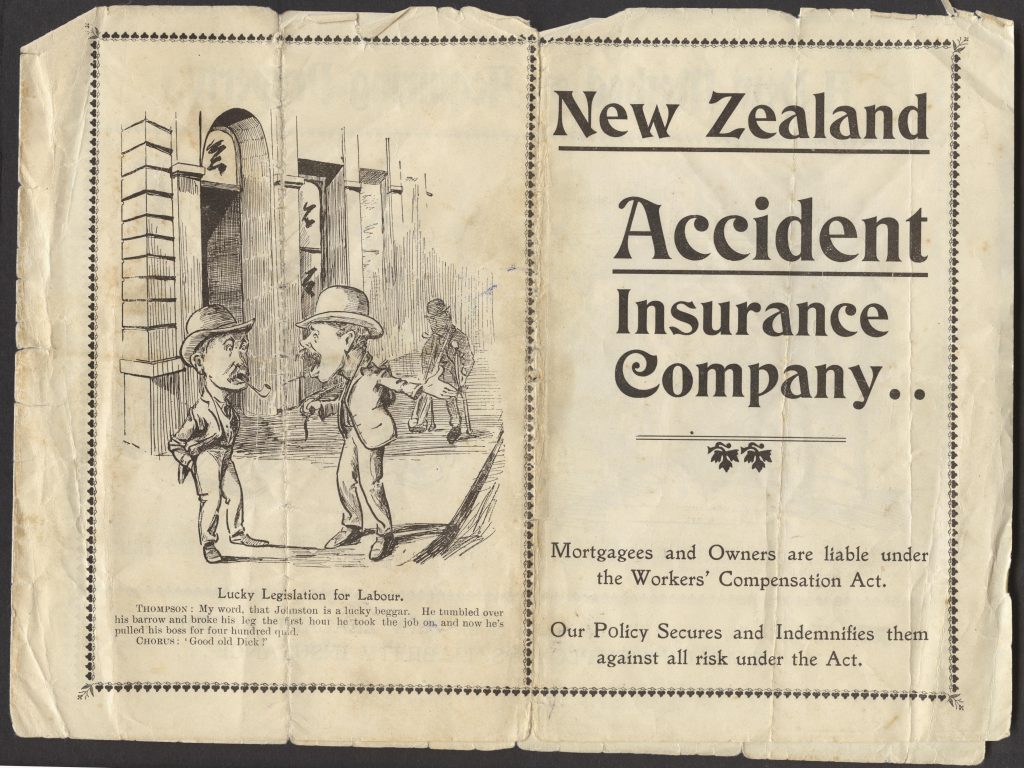 If you are injured on the job, you might be entitled to compensation through the workers’ compensation system. What happens if your employer denies your claims for treatment recommended by your treating physicians? Can your employer be required to pay you penalties and fees?
If you are injured on the job, you might be entitled to compensation through the workers’ compensation system. What happens if your employer denies your claims for treatment recommended by your treating physicians? Can your employer be required to pay you penalties and fees? While involved in a legal dispute, there are strict timelines that must be followed, not only for filing an initial lawsuit, but also for filing any subsequent appeals. However, arguments can arise about what timeline applies to a certain factual situation.
While involved in a legal dispute, there are strict timelines that must be followed, not only for filing an initial lawsuit, but also for filing any subsequent appeals. However, arguments can arise about what timeline applies to a certain factual situation.  Honesty is the best policy. This is especially true in the workers’ compensation space, because if you are found to have been fraudulent, you forfeit your right to workers’ compensation benefits.
Honesty is the best policy. This is especially true in the workers’ compensation space, because if you are found to have been fraudulent, you forfeit your right to workers’ compensation benefits.  When receiving medical care, the choice of medical professional can influence your treatment. If you have been injured on the job, you might not be sure if you can pick your own doctor or if you have to use a doctor your employer selects. Under the Louisiana Workers’ Compensation Act, an injured worker is entitled to select a physician in any specialty for an initial visit. The employer is not required to approve the employee’s choice of physician. What happens if the employer claims the employee was not injured on the job?
When receiving medical care, the choice of medical professional can influence your treatment. If you have been injured on the job, you might not be sure if you can pick your own doctor or if you have to use a doctor your employer selects. Under the Louisiana Workers’ Compensation Act, an injured worker is entitled to select a physician in any specialty for an initial visit. The employer is not required to approve the employee’s choice of physician. What happens if the employer claims the employee was not injured on the job?